A dance-fitness program adapted for expectant mothers is a modified version of a popular exercise class. The adaptations account for the physiological changes and specific safety considerations unique to gestation, aiming to provide a safe and effective means of physical activity. An example is a class that reduces high-impact movements, incorporating modified choreography to accommodate balance shifts and joint flexibility changes common during pregnancy.
Its significance lies in offering a low-to-moderate intensity cardiovascular workout, potentially promoting cardiovascular health, maintaining weight, and improving mood during gestation. Historically, the incorporation of exercise during pregnancy has evolved as research supports its benefits, with specialized classes becoming increasingly prevalent as a safe and social outlet for expectant mothers. Benefits may include improved sleep, reduced back pain, and preparation for labor and delivery.
The subsequent sections will address key considerations for participation, contraindications, and modifications necessary to ensure maternal and fetal well-being. These considerations are paramount in maximizing benefits while mitigating potential risks associated with physical activity during gestation.
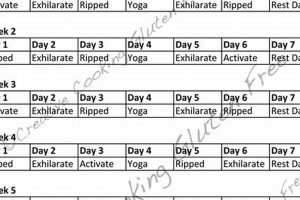
Guidance for Modified Dance-Fitness During Gestation
This section outlines important considerations for engaging in a modified dance-fitness program during pregnancy to ensure safety and efficacy. Prior consultation with a qualified healthcare provider is essential before commencing any exercise regimen during gestation.
Tip 1: Maintain Adequate Hydration: Dehydration can lead to complications during pregnancy. Consume sufficient fluids before, during, and after participation.
Tip 2: Monitor Exercise Intensity: Adhere to a perceived exertion level that allows for comfortable conversation. Breathlessness or lightheadedness indicates excessive exertion.
Tip 3: Modify High-Impact Movements: Replace jumping, hopping, and rapid changes in direction with low-impact alternatives. This minimizes stress on joints and the pelvic floor.
Tip 4: Avoid Supine Positions After the First Trimester: Lying flat on the back can compress the vena cava, reducing blood flow to the uterus. Modify exercises to a seated or side-lying position.
Tip 5: Listen to the Body: Discontinue exercise immediately upon experiencing pain, dizziness, vaginal bleeding, or contractions. Seek medical advice promptly if these symptoms occur.
Tip 6: Wear Appropriate Attire: Supportive athletic shoes and comfortable clothing that allows for freedom of movement are essential. Consider a supportive maternity belt if experiencing lower back pain.
Tip 7: Ensure Adequate Warm-up and Cool-down: Begin with a gentle warm-up to prepare muscles for activity and end with a cool-down to gradually decrease heart rate. Static stretching should be performed after the cool-down.
Adhering to these guidelines promotes a safer and more beneficial exercise experience during pregnancy, potentially enhancing physical and mental well-being. Individual responses to exercise can vary; therefore, close monitoring and adjustment of the exercise routine are crucial.
The subsequent section will address specific modifications to common dance-fitness moves and scenarios where participation is contraindicated. This comprehensive approach supports informed decision-making regarding physical activity during gestation.
1. Modified Movements
In the context of dance-fitness for pregnant individuals, the principle of “Modified Movements” is paramount. It ensures that the physical demands of the activity align with the physiological changes and safety considerations inherent in gestation, making it an accessible and beneficial form of exercise.
- Impact Reduction
This involves replacing high-impact actions like jumping, hopping, and plyometrics with low-impact alternatives such as stepping, marching, or swaying. Reducing impact minimizes stress on joints, particularly the knees, ankles, and pelvic floor, which are more vulnerable during pregnancy due to hormonal changes and increased weight. For example, instead of a jumping jack, a participant might perform a lateral step with arm movements.
- Range of Motion Adjustments
During pregnancy, the hormone relaxin increases joint laxity, making individuals more susceptible to sprains and strains. Modified Movements address this by reducing the range of motion in certain exercises. For instance, deep squats may be modified to partial squats, and wide stances may be narrowed to maintain stability. This helps prevent overextension and potential injury.
- Balance and Stability Enhancements
As the center of gravity shifts during pregnancy, balance can be compromised. Modified Movements incorporate exercises that enhance stability, such as utilizing a wider base of support, engaging core muscles (when appropriate and safe), and performing movements in a controlled manner. Examples include slow, deliberate steps and the use of stable surfaces for support if needed.
- Core Engagement Adaptations
While traditional core exercises may be contraindicated during pregnancy, Modified Movements focus on engaging the deep core muscles in a safe and effective way. This may involve pelvic tilts, gentle abdominal contractions, and diaphragmatic breathing. These techniques help maintain core stability and support the spine without putting excessive strain on the abdominal muscles. Emphasis is placed on avoiding exercises that cause coning or doming of the abdomen.
The integration of these facets of “Modified Movements” within a dance-fitness routine allows pregnant individuals to derive the cardiovascular and mood-boosting benefits of exercise while minimizing risks. The adaptations account for the specific needs of the pregnant body, promoting a safe and enjoyable experience. These movement adjustments are crucial for maximizing benefits and decreasing potential dangers related to activity throughout gestation.
2. Hydration Strategies
Effective “Hydration Strategies” are a critical component of a modified dance-fitness program for expectant mothers, as pregnancy inherently increases fluid requirements. The physiological changes during gestation, including increased blood volume and amniotic fluid production, elevate the risk of dehydration. Participation in physical activity further exacerbates this risk through sweat loss. Inadequate hydration can lead to decreased blood flow to the uterus, potentially affecting fetal well-being. A practical example includes a pregnant individual experiencing premature contractions due to dehydration following a class. Proper fluid intake before, during, and after physical activity helps maintain blood volume, regulate body temperature, and facilitate nutrient transport to both the mother and fetus.
Specific recommendations for fluid intake during participation depend on individual factors such as metabolic rate, ambient temperature, and exercise intensity. However, a general guideline involves consuming water before the session, sipping fluids every 15-20 minutes during the activity, and replenishing fluids post-exercise. Electrolyte-containing beverages may be considered during longer or more intense sessions to replace sodium and potassium lost through sweat. Monitoring urine color can serve as a practical indicator of hydration status; pale yellow urine generally signifies adequate hydration, while dark yellow urine indicates dehydration.
Therefore, integrating structured “Hydration Strategies” into a modified dance-fitness regimen for expectant mothers is essential for ensuring maternal and fetal health. Neglecting this aspect can negate the potential benefits of exercise and increase the risk of adverse outcomes. Adherence to a well-planned hydration protocol requires education, consistent monitoring, and individual adjustments based on physiological responses.
3. Intensity Regulation
Intensity regulation, within the context of adapted dance-fitness for pregnant individuals, is the mindful control and modification of exertion levels during physical activity. The physiological adaptations to pregnancy impact cardiovascular and respiratory systems; therefore, uncontrolled or excessive intensity poses potential risks to both mother and fetus. Elevated maternal heart rate can reduce uterine blood flow, potentially compromising fetal oxygen supply. Overexertion may also trigger premature contractions or exacerbate existing pregnancy-related discomforts. Consequently, intensity regulation serves as a crucial safeguard within a modified dance-fitness program.
Practical application involves monitoring perceived exertion using scales such as the Borg Rating of Perceived Exertion (RPE). Encouraging participants to maintain an RPE level that allows for comfortable conversation is a common strategy. Modifications include reducing the amplitude of movements, decreasing the speed of the choreography, and incorporating rest periods. For instance, a participant who experiences shortness of breath during a sequence may modify the step pattern to a less demanding variation or temporarily reduce participation. Educating participants on the importance of self-monitoring and responding appropriately to physiological cues is integral to safe and effective intensity regulation.
In conclusion, appropriate intensity regulation is not merely an ancillary consideration but a core component of a safe and beneficial dance-fitness experience during pregnancy. Ignoring or mismanaging exertion levels can undermine the potential benefits of physical activity and increase the risk of adverse events. The challenge lies in providing instruction that is adaptable, empowering participants to take ownership of their exertion levels and make informed modifications to ensure both maternal and fetal well-being. The proper application and monitoring of intensity regulation creates a positive and productive class experience for expectant mothers.
4. Physician Clearance
Prior medical authorization represents a fundamental prerequisite for participation in a modified dance-fitness program during gestation. This step ensures that pre-existing conditions or pregnancy-related complications are identified and addressed, minimizing potential risks associated with physical exertion.
- Risk Stratification
The primary function of medical evaluation lies in stratifying individuals based on their risk profile. Obstetricians assess factors such as pre-existing cardiovascular disease, gestational diabetes, placenta previa, or a history of preterm labor. Individuals with high-risk pregnancies may be advised to avoid exercise or engage in highly modified activities under close medical supervision. This targeted approach minimizes potential harm.
- Activity Recommendation Tailoring
Medical assessment facilitates tailored recommendations regarding appropriate exercise types, intensity, and duration. For example, an individual with well-controlled gestational diabetes may receive clearance for moderate-intensity dance-fitness, coupled with specific guidelines for monitoring blood glucose levels. Conversely, someone with uncontrolled hypertension may be advised against high-impact activities. The customization enhances safety and effectiveness.
- Symptom Management Guidance
Medical professionals can provide guidance on managing common pregnancy-related symptoms that may be exacerbated by exercise. These symptoms include shortness of breath, pelvic pain, and edema. Clear communication between the pregnant individual, healthcare provider, and fitness instructor ensures appropriate modifications are implemented to mitigate discomfort and prevent adverse events.
- Legal and Ethical Considerations
Requiring medical clearance mitigates legal liability for fitness instructors and facilities. It establishes a documented process demonstrating due diligence in safeguarding participants’ well-being. From an ethical standpoint, prioritizing the health and safety of pregnant individuals aligns with professional standards within both the medical and fitness communities.
The facets outlined above underscore the integral role of physician authorization in the context of modified dance-fitness during gestation. This process is not merely a formality but a crucial safeguard that enhances safety, promotes personalized recommendations, and mitigates potential risks. Integrating this requirement ensures that participation is appropriate and beneficial for both mother and fetus.
5. Postpartum Transition
The postpartum period, characterized by significant physiological and psychological adjustments following childbirth, necessitates a carefully considered approach to resuming physical activity. Prior engagement in a modified dance-fitness program during gestation can influence the ease and safety of this transition, provided appropriate guidelines are followed.
- Pelvic Floor Rehabilitation
Pregnancy and childbirth often weaken pelvic floor muscles, leading to urinary incontinence or pelvic organ prolapse. A gradual return to activity post delivery is crucial. A pre-existing awareness of proper pelvic floor engagement, potentially developed during prenatal classes, can inform a more effective rehabilitation strategy. Activities should initially focus on strengthening these muscles before reintroducing impact exercises.
- Abdominal Muscle Recovery
Diastasis recti, the separation of abdominal muscles, is common during pregnancy. Premature or aggressive abdominal exercises post childbirth can exacerbate this condition. An understanding of appropriate core engagement, ideally established during a prenatal program, guides a safe return to abdominal strengthening. Exercises should prioritize deep core activation before progressing to more challenging movements.
- Gradual Cardiovascular Resumption
Cardiovascular fitness may decline during pregnancy and immediately postpartum. A measured return to dance-fitness activities is advisable, starting with low-intensity sessions and gradually increasing duration and intensity. Monitoring heart rate and perceived exertion is crucial to avoid overexertion, which could impede recovery or affect lactation.
- Psychological Adaptation and Social Support
The postpartum period is often associated with emotional and psychological challenges. Engaging in dance-fitness can provide a sense of normalcy and promote mental well-being. Continued participation in a supportive class environment, potentially carried over from the prenatal period, can offer valuable social support and reduce feelings of isolation.
These facets highlight the interconnectedness between prenatal physical activity and the postpartum recovery process. While prenatal participation in a modified dance-fitness program offers potential advantages, a cautious and individualized approach is paramount. Medical clearance and guidance from qualified healthcare professionals are essential to ensure a safe and effective transition back to physical activity.
Frequently Asked Questions
The following section addresses common inquiries regarding modified dance-fitness during gestation, aiming to provide clarity and evidence-based information.
Question 1: Is modified dance-fitness safe during all trimesters of pregnancy?
Safety depends on individual health status and pregnancy-specific factors. Medical clearance is required prior to participation. Modifications are necessary to accommodate changing physiological needs across trimesters.
Question 2: What specific modifications are implemented to ensure safety?
Modifications include reducing high-impact movements, adjusting range of motion, maintaining adequate hydration, and carefully regulating exercise intensity. Avoidance of supine positions after the first trimester is also crucial.
Question 3: Are there any contraindications for engaging in modified dance-fitness during pregnancy?
Contraindications may include pre-existing cardiovascular disease, placenta previa, uncontrolled hypertension, a history of preterm labor, or other pregnancy-related complications. A healthcare provider can assess individual risk factors.
Question 4: How does intensity regulation affect the efficacy of this workout?
Appropriate intensity regulation optimizes cardiovascular benefits while minimizing risks. Perceived exertion levels should allow for comfortable conversation, and exercises should be modified as needed to prevent overexertion.
Question 5: What are the benefits of incorporating hydration strategies during this activity?
Adequate hydration maintains blood volume, regulates body temperature, and facilitates nutrient transport to both the mother and fetus. Dehydration can lead to decreased uterine blood flow and potential complications.
Question 6: How should an individual transition back to regular exercise postpartum after participating in modified dance-fitness during pregnancy?
The postpartum transition should be gradual, focusing initially on pelvic floor rehabilitation and abdominal muscle recovery. Medical clearance and guidance from healthcare professionals are essential to ensure a safe and effective return to physical activity.
Adherence to guidelines, including physician authorization, modified movements, and intensity regulation, is essential for maximizing benefits and minimizing risks. Each woman needs to customize the training for a better result.
The subsequent section will summarize key recommendations for engaging in adapted dance-fitness, emphasizing the importance of personalized care and informed decision-making.
Considerations for Safe and Effective Dance-Fitness During Gestation
The preceding exposition has detailed crucial aspects of adapted dance-fitness for expectant mothers. Key points include the necessity of physician clearance, the implementation of modified movements to accommodate physiological changes, the importance of hydration strategies, and the careful regulation of exercise intensity. Successfully navigating exercise during this period demands a comprehensive understanding of individual health status, pregnancy-specific risks, and appropriate modification techniques. Failure to address these factors may negate potential benefits and increase the likelihood of adverse events.
In summation, safe and effective participation in zumba pregnancy workout requires an informed and cautious approach. Prioritizing maternal and fetal well-being, adhering to medical guidance, and engaging in mindful self-monitoring are paramount. Ongoing research and clinical experience continue to refine best practices in this domain. Expectant mothers are encouraged to engage in open dialogue with healthcare providers and qualified fitness professionals to ensure a personalized and evidence-based approach to physical activity during this transformative period.